Diagnosis & Imaging
Imaging
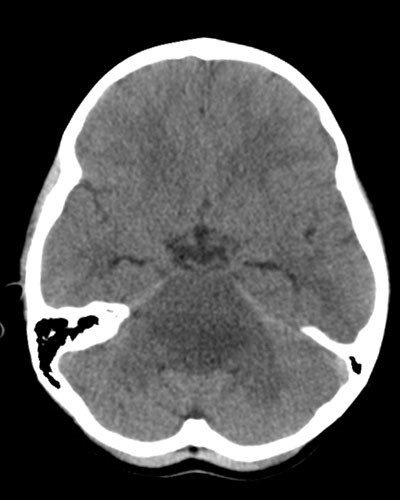
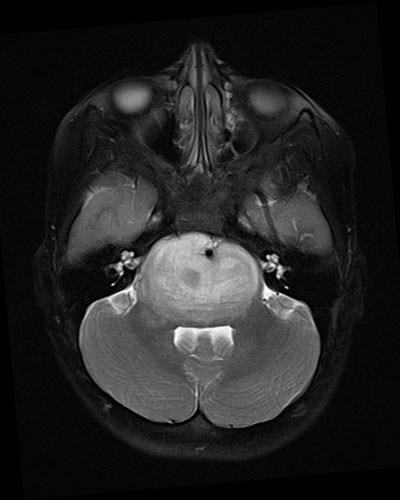
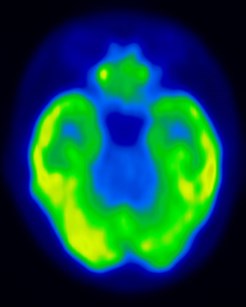
Imaging is the primary diagnostic tool for DIPG. CT is often the first exam obtained, as it can be quickly performed without sedation/anesthesia. It will usually show a low-density expansion of the pons with flattening of the fourth ventricle. However, some lesions are extremely subtle on CT, and MR imaging is the preferred diagnostic modality. MR typically shows a diffuse expansion of the brainstem/pons by a tumor that is poorly defined but abnormally bright in signal on T2-weighted images and abnormally dark on T1-weighted images. Contrast enhancement is seen in the minority of DIPG, and when present is typically mild. There may be some indication of necrosis, and the basilar artery is commonly engulfed by tumor. Hemorrhage and calcification are uncommon.
|
|
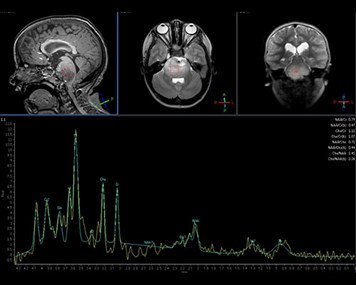
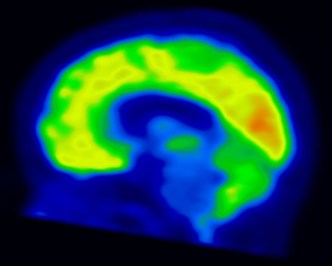
MR spectroscopy may be helpful in distinguishing tumor from brainstem encephalitis, and may have a role inguidingbiopsy or evaluating response to therapy. PET scans have been used in some cases to guide biopsy. Surveillance MR imaging can be used to monitor response to therapy and progression of disease, however clinical assessment is usually much more reliable.
 |
 |
 |
Role of Biopsy
Because diagnosis can generally be made on the basis of clinical presentation and imaging, and because histological findings have not historically guided treatment, surgical biopsy has rarely been employed, in part because of the perceived risk of morbidity, specifically in North America.1,2 Biopsy is usually performed when either neurological findings, duration of symptoms or imaging studies are atypical or inconclusive.
More recent studies have suggested that stereotactic needle biopsy has no mortality and a low risk of morbidity.3-5 A biopsy, in the context of a classical DIPG, seems most defensible if subsequent treatment will be tailored accordingly. At some primarily European centers, stereotactic needle biopsy is now more widely used to confirm diagnosis when either neurological findings or imaging studies are atypical or inconclusive.
This is the concept of a recent trial, led by Dr. Mark Kieran/Boston Childrens Hospital. Children diagnosed with DIPG undergo biopsy for stratification to 3 different treatment arms. The study is ongoing, and over 20 centers in the US are participating (NCT01182350). Based on these data, stereotactic biopsy for patients with DIPG appears feasible, safe, and diagnostic for molecular analysis. As targeted therapies become available, it is hoped that the molecular profile of the tumor may aid determining effective tailored treatment regimen.
Because the scarcity of tumor samples has hampered research on the genetics and biology of DIPG, patients who have undergone surgical biopsy and their families should be advised of the opportunity to donate leftover tissue to the International DIPG Registry and/or other research projects or tissue banks.
- References
1. Epstein, F. and E.L. McCleary, Intrinsic brain-stem tumors of childhood: Surgical indications. Journal of neurosurgery, 1986. 64(1): p. 11-5. - Jansen, M.H., et al., Diffuse intrinsic pontine gliomas: A systematic update on clinical trials and biology. Cancer treatment reviews, 2012. 38(1): p. 27-35.
- Cartmill, M. and J. Punt, Diffuse brain stem glioma. A review of stereotactic biopsies. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery, 1999. 15(5): p. 235-7; discussion 238.
- Pincus, D.W., et al., Brainstem stereotactic biopsy sampling in children. Journal of neurosurgery, 2006. 104(2 Suppl): p. 108-14.
- Roujeau, T., et al., Stereotactic biopsy of diffuse pontine lesions in children. Journal of neurosurgery, 2007. 107(1 Suppl): p. 1-4.
- Puget, S., et al., Mesenchymal transition and PDGFRA amplification/mutation are key distinct oncogenic events in pediatric diffuse intrinsic pontine gliomas. PLoS One, 2012.
